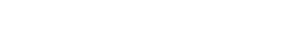
Obesity is the first thing you see. Don’t make it the last thing you talk about
Obesity is associated with at least 60 comorbidities, some of which can be improved through weight loss.1-4
While the majority of patients and HCPs agree that weight loss of 10% may be beneficial to their health, patients may be waiting for HCPs to take that important first step and discuss weight management.5*
*Data from a survey that examined obesity-related perceptions, attitude, and behaviors among ~3,000 adults with obesity and ~600 HCPs.
It’s time to bring obesity to the forefront
Weight-related comorbidities are just that: medical conditions that may often be associated with obesity.
Weight loss of 5% to 15% or greater may result in improvements in many of these comorbidities2:
- Patients with obesity and depression interested in weight loss should be offered structured lifestyle intervention3
- Weight loss of 5% to 10% may reduce the risk for emergent depression2
- It is estimated that nearly half of all people with obesity also have obstructive sleep apnea6
- Weight loss of 10% or more can significantly improve apnea hypopnea index in OSA2
- Patients with obesity and GERD should be treated for weight loss. In these patients, the weight-loss goal should be 10% of body weight or greater3
Obesity is associated with many common CVD risk factors, including7:
- Hypertension
- Dyslipidemia
- Type 2 diabetes
- Patients with obesity and asthma should be treated with weight loss using lifestyle interventions but additional treatment modalities may be considered. For these patients, the weight-loss goal should be at least 7% to 8%3
- A systematic review and meta-analysis reveal that NAFLD was present in nearly 60% of patients with obesity8
- Waist circumference—more than elevated BMI—can increase risk for NAFLD9
- Weight loss of 5% to 10% improves symptoms in men and women3
- Weight loss of 2.5% to <15% improves glycemic control; greater weight loss is associated with greater glycemic improvement2
- With a 5% to 15% weight loss, patients with obesity can improve certain PCOS symptoms, such as hyperandrogenism, oligomenorrhea, and anovulation3
- Weight loss of more than 5% to 10% is needed for significant improvement in serum testosterone3
- Weight loss of 5% to 10% improves knee functionality, pain, walking distance, and speed2
- Weight loss of 2% to 5% improves ovulatory cycle, with more weight loss producing a more robust effect2
- Metabolic syndrome is characterized by the concurrent presence of at least 3 of 5 specific conditions: abdominal obesity, raised triglycerides, low HDL cholesterol, elevated blood pressure, and elevated blood glucose10
- Weight loss of 2.5% to 10% can prevent diabetes in impaired glucose tolerance2
- Weight loss of 2.5% to <15% is associated with lower triglycerides2
- Weight loss of 5% to <15% is associated with HDL increase (not true for BMI >40)2
- Weight loss of 5% to 10% was shown to increase odds of achieving a 5 mm Hg reduction in both systolic and diastolic blood pressure in a study of 5,145 patients with overweight or obesity and type 2 diabetes11
- 13 cancers are associated with excess weight and obesity4
- About 40% of all cancers diagnosed in the US have been associated with overweight and obesity4
Weight loss can help improve some of your patients' weight-related comorbidities
For a deeper look into some of these conditions, tap on each weight-related comorbidity to explore the role obesity can play in your patients’ health.
Cardiovascular disease
Nonalcoholic fatty liver disease (NAFLD)
Polycystic ovary syndrome (PCOS)
Osteoarthritis (OA)

Prediabetes
Obstructive sleep apnea (OSA)

Comorbidities of obesity brochure
This brochure includes an overview of some common weight-related comorbidities and the impact weight loss may have on them.
Obesity is caused by a range of factors
Patients may be waiting for HCPs to take that important first step and discuss weight management
References
1. Bays HE, McCarthy W, Christensen S, et al. Obesity algorithm 2020. Presented by the Obesity Medicine Association. Accessed November 21, 2022. https://obesitymedicine.org/obesity-algorithm
2. Ryan DH, Yockey SR. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Curr Obes Rep. 2017;6(2):187-194.
3. Garvey WT, Mechanick JI, Brett EM; and Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(suppl 3):1-203.
4. Cancers associated with overweight and obesity make up 40 percent of cancers diagnosed in the United States. Centers for Disease Control and Prevention. Accessed November 22, 2022. https://www.cdc.gov/media/releases/2017/p1003-vs-cancer-obesity.html
5. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the national ACTION study. Obesity (Silver Spring). 2018;26(1):61-69.
6. Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010;137(3):711-719.
7. Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143(21):e984-e1010.
8. Le MH, Yeo YH, Li X, et al. 2019 global NAFLD prevalence: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2022;20(12):2809-2817.e28.
9. Cotter TG, Rinella M. NAFLD 2020: the state of the disease. Gastroenterology. 2020;158(7):1851-1864.
10. Metabolic syndrome. Mayoclinic.org. Accessed November 24, 2020. https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916
11. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Care. 2011;34(7):1481-1486.