Physiology of weight loss
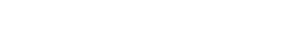
A physiological tug-of-war: weight loss via reduced-calorie intake triggers the process of metabolic adaptation in the brain and body.1,2
Metabolic and hormonal responses affect patients‘ ability to maintain weight loss1
Weight loss due to calorie restriction may cause the body to react by slowing metabolism and altering appetite-regulating hormones in a process called metabolic adaptation, making long-term weight management difficult.1,2
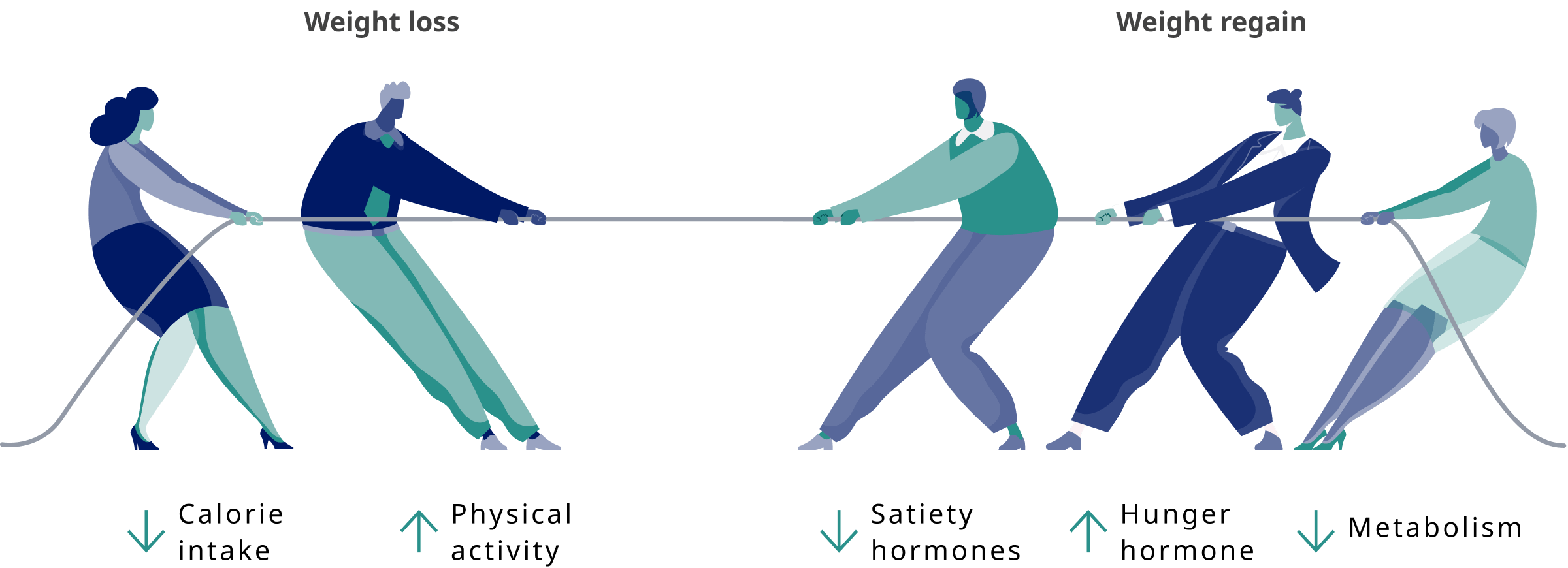
Which hormones are affected by metabolic adaptation?1
After weight loss via reduced-calorie intake, metabolic adaptation may result in increased signals for energy intake (increase in the hunger hormone [ie, ghrelin] and decrease in satiety hormones [eg, GLP-1, PYY, CCK, amylin]).
Study Design
Study enrolled 50 overweight or obese patients without diabetes in a 10-week weight-loss program, with a very-low-energy diet prescribed. The circulating levels of leptin, ghrelin, peptide YY, gastric inhibitory polypeptide, glucagon-like peptide-1, amylin, pancreatic polypeptide, cholecystokinin, insulin, and subjective ratings of appetite were examined at baseline (before weight loss), at 10 weeks (after program completion), and at 62 weeks.1
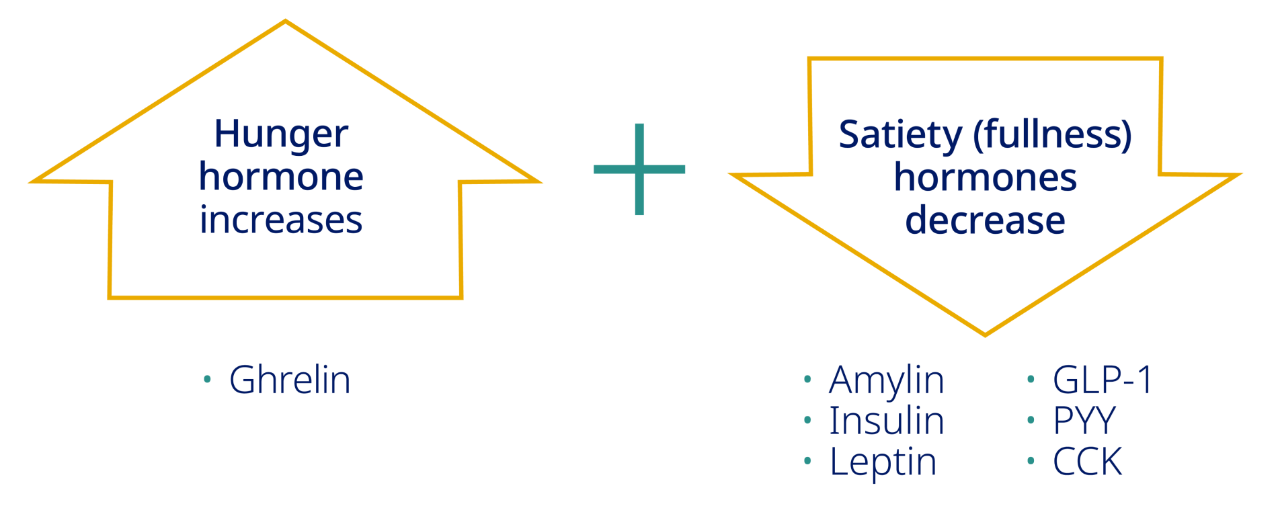
The brain plays a critical role in appetite regulation5-10
For people with obesity trying to lose weight and maintain it, hunger that drives increased eating is a major challenge.5-10
Learn more about the brain's key role in appetite regulation
Watch how GLP-1 works to regulate appetite
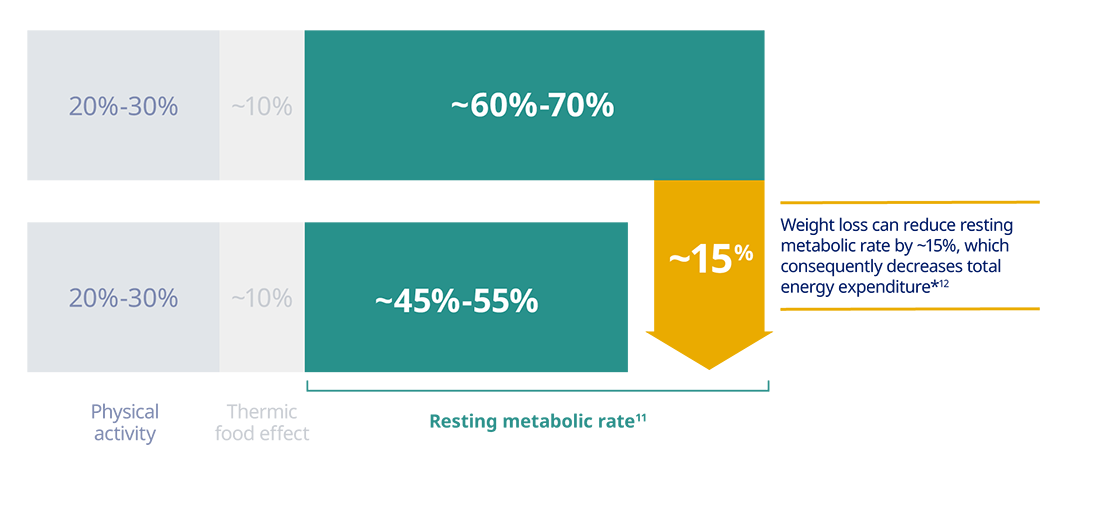
After weight loss, metabolic adaptation leads to decreases in resting metabolic rate and lower energy expenditure2
The majority of energy expenditure comes from resting metabolic rate.2,11
Study Design
A review of data from indirect calorimetry to gain insights into the determinants of energy metabolism and its role in weight gain, and therefore the use of such method to combat obesity.11
*Data from a two-part study where 20 subjects underwent an 11-week weight-loss program. Results observed after fat mass loss of 15% of baseline.12
When people with obesity try to lose weight, metabolic adaptation will counteract their weight-loss efforts. Metabolic adaptations must be continuously offset through long-term weight management.1,13,14

Obesity treatment case studies
Review case studies about patients with obesity that may be similar to patients you see in your own practice.

Looking beyond the scale
In this video, Dr. Holly Lofton challenges current thinking when it comes to treating patients with obesity and discusses metabolic adaptation after weight loss.
Obesity is a relapsing disease
Pharmacotherapy may help patients keep weight off
References
1. Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365(17):1597-1604.
2. Lam YY, Ravussin E. Analysis of energy metabolism in humans: a review of methodologies. Mol Metab. 2016;5(11):1057-1071.
3. Metabolic syndrome. Mayo Clinic. Accessed March 1, 2021. https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916
4. Hall KD, Kahan S. Maintenance of lost weight and long-term management of obesity. Med Clin North Am. 2018;102(1):183-197.
5. Yu JH, Kim MS. Molecular mechanisms of appetite regulation. Diabetes Metab J. 2012;36(6):391-398.
6. Austin J, Marks D. Hormonal regulators of appetite. Int J Pediatr Endocrinol. 2009;2009:141753.
7. Guyenet SJ, Schwartz MW. Clinical review: Regulation of food intake, energy balance, and body fat mass: implications for the pathogenesis and treatment of obesity. J Clin Endocrinol Metab. 2012;97(3):745-755.
8. Farr OM, Li CR, Mantzoros CS. Central nervous system regulation of eating: Insights from human brain imaging. Metabolism. 2016;65(5):699-713.
9. Cassidy RM, Tong Q. Hunger and satiety gauge reward sensitivity. Front Endocrinol (Lausanne). 2017;8:104.
10. Druce MR, Small CJ, Bloom SR. Minireview: gut peptides regulating satiety. Endocrinology. 2004;145(6):2660-2665.
11. Lam YY, Ravussin E. Indirect calorimetry an indispensable tool to understand and predict obesity. Eur J C!in Nutr. 2017;71(3):318-322.
12. Connolly J, Romano T, Patruno M. Selections from current literature: effects of dieting and exercise on resting metabolic rate and implications for weight management. Fam Pract. 1999;16(2):196-201.
13. Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease. A position statement of the World Obesity Federation. Obes Rev. 2017;18(7):715-723.
14. Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(suppl 3):1-203.