RESOURCE LIBRARY
Download materials to support your conversations with people living with obesity

Comorbidities of obesity brochure
This brochure includes an overview of common weight-related comorbidities and the impact weight loss may have on them.
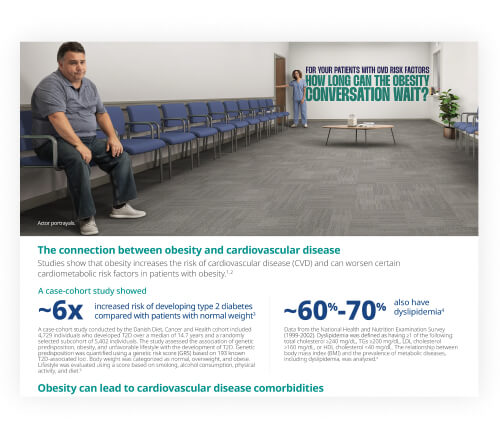
Obesity and cardiovascular disease flash card
Learn more about the connection between obesity and cardiovascular disease.

Metabolic adaptation flash card
This resource discusses the mechanisms that contribute to weight regain.
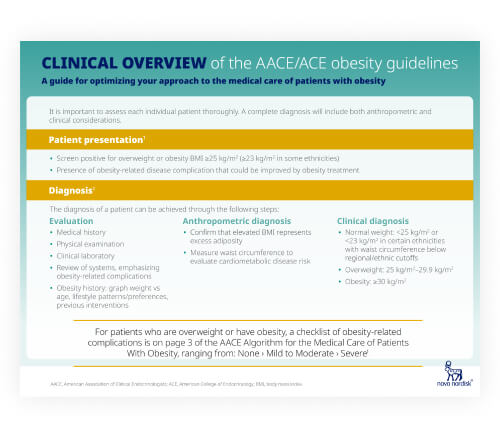
Overview of the AACE/ACE obesity guidelines
Obesity is recognized as a chronic, progressive disease. Check out the full guidelines for details on how to treat.
Additional resources for you
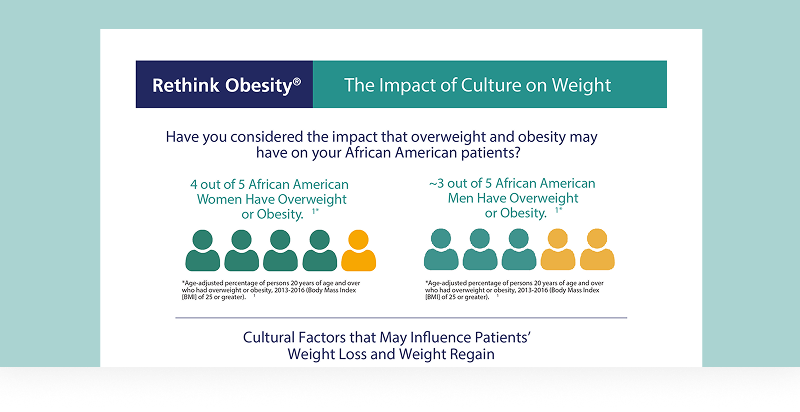
The impact of culture on weight flash card
Understand how cultural factors may impact weight management.
Importance of early diagnosis flash card
See how early diagnosis of obesity may help improve patients' weight and health outcomes.

Obesity and CVD risk patient identification guide
Explore key information to consider when evaluating CVD risk for your patients with obesity.

Providing a comfortable environment for patients with obesity flash card
Review tips to help promote a comfortable environment for your patients with obesity.
AACE, American Association of Clinical Endocrinology; ACE, American College of Endocrinology; CVD, cardiovascular disease.
Watch these videos to better understand other health care professionals' approach toward patients living with obesity and long-term weight management
Moving the Conversation From Blame to Biology
Dr. Campos talks about how he approaches patients with obesity with partnership and compassion.
The Tug-of-War in the Body
Dr. Lofton explains how metabolic adaptation creates a battle between weight loss and regain.

The Constellation of Risks of Obesity
Dr. Rajper speaks about how he approaches patients with obesity as a cardiologist.
Words Matter in the Obesity Conversation
Dr. Sobel shares how you speak about obesity can affect your patients.
Reframing Obesity Management
Dr. Holly Lofton discusses how obesity is often managed differently than other chronic diseases and highlights the need for proper diagnosis and treatment.
Exploring Weight-Related Comorbidities
Dr. Carlos Campos discusses the association between obesity and weight-related comorbidities, highlighting potential approaches to guide effective weight-management discussions with patients.
The Importance of Assessing Cardiovascular Risk

The Science Behind Obesity
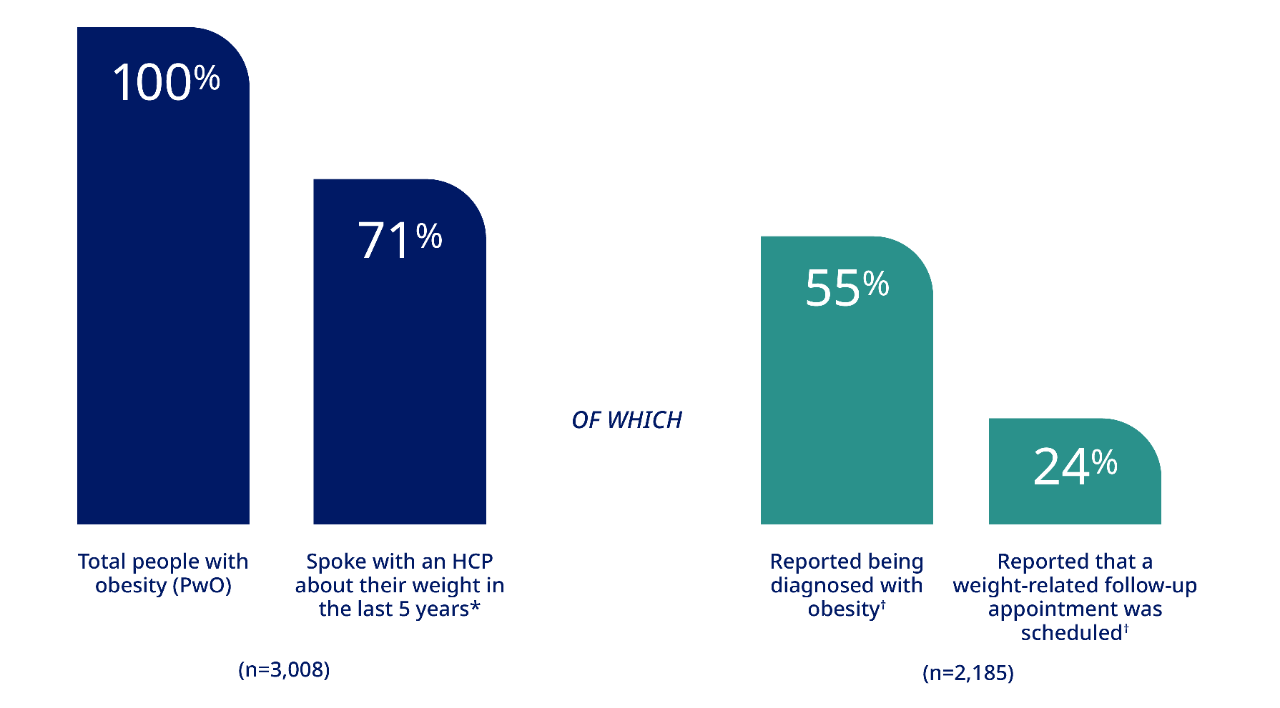
The ACTION Study
The ACTION (Awareness, Care and Treatment In Obesity MaNagement) Study is the first multidisciplinary study to explore the barriers and perspectives on obesity among 3 important groups in the sphere of obesity care: People with obesity, health care professionals, and employers.
Conversations about weight are insufficient
ACTION Study identifies 5 key barriers to obesity care*

Weight-loss challenges1
- People with obesity engage in an average of 7 serious weight-loss attempts
- 23% reported a 10% weight loss in the last 3 years
- Of these, 44% were able to maintain the weight loss for more than 1 year (10% of total sample)

Reluctance to seek help1
- Despite recognition of obesity as a disease, 82% of people with obesity consider weight loss to be completely their own responsibility
- This may prevent them from seeking help from their health care professional
Lack of diagnosis1
- Only 55% of people with obesity have received a formal diagnosis of obesity
- Health care professionals inconsistently record diagnosis of obesity

Inadequate follow-up1
- 52% of HCPs report that they lack time in appointments to discuss obesity and 45% say there are more important issues to discuss
- 24% of patients with obesity say a follow-up to discuss obesity was scheduled
Unclear wellness offerings1
- 72% of employers perceive their wellness programs offer benefit
- Only 17% of employees with obesity agree
*The first US nationwide study to investigate barriers to obesity management from the perspective of people with obesity, health care professionals, and employers, the ACTION Study quantitative research follows a literature review and robust qualitative research. The data were collected through surveys of more than 3,000 people with obesity, 600 health care professionals, and 150 employers.
1. Kaplan LM, Golden A, Jinnett K, et al. Perceptions of barriers to effective obesity care: results from the National ACTION Study. Obesity (Silver Spring). 2018;26(1):61-69.