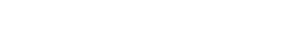
Metabolic adaptation can make sustained weight loss difficult
Weight loss via reduced-calorie intake triggers metabolic adaptation in both the brain and body.1,2
Sustained weight loss can be challenging due to the natural process of metabolic adaptation1,2
Even if adults achieve weight loss with reduced-calorie intake, metabolic adaptation and changes in appetite-regulating hormones drive weight regain, making long-term weight management very challenging.1,2
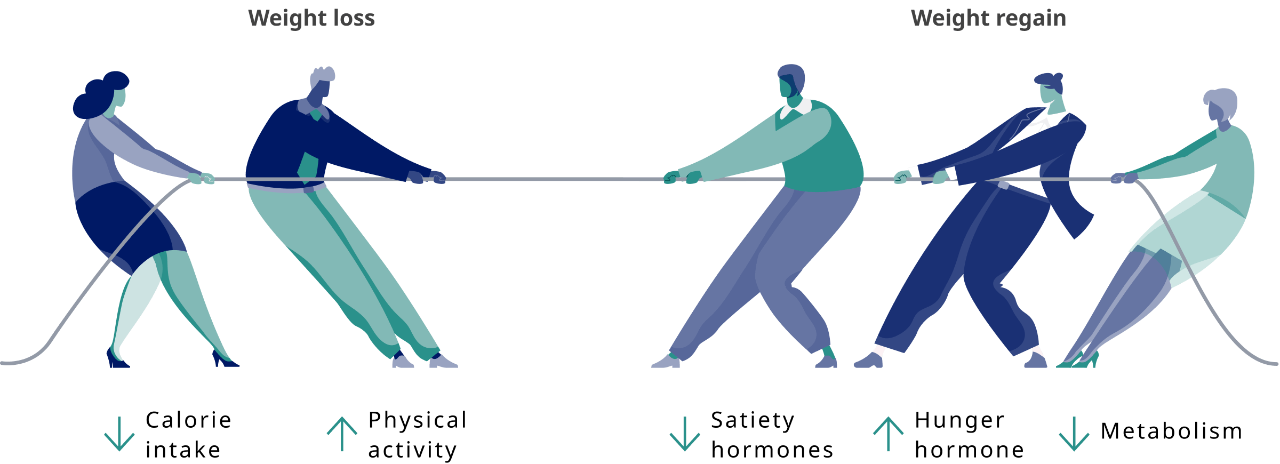
Which hormones are affected by metabolic adaptation?
After weight loss via reduced-calorie intake, metabolic adaptation may result in increased signals for energy intake (increase in the hunger hormone [ie, ghrelin] and decrease in satiety hormones [eg, GLP-1, PYY, CCK, amylin]).1
Study Design
Study enrolled 50 adults with overweight or obesity, without diabetes, in a 10-week weight-loss program, with a very-low-energy diet prescribed. The circulating levels of leptin, ghrelin, peptide YY, gastric inhibitory polypeptide, GLP-1, amylin, pancreatic polypeptide, cholecystokinin, insulin, and subjective ratings of appetite were examined at baseline (before weight loss), at 10 weeks (after program completion), and at 62 weeks.1
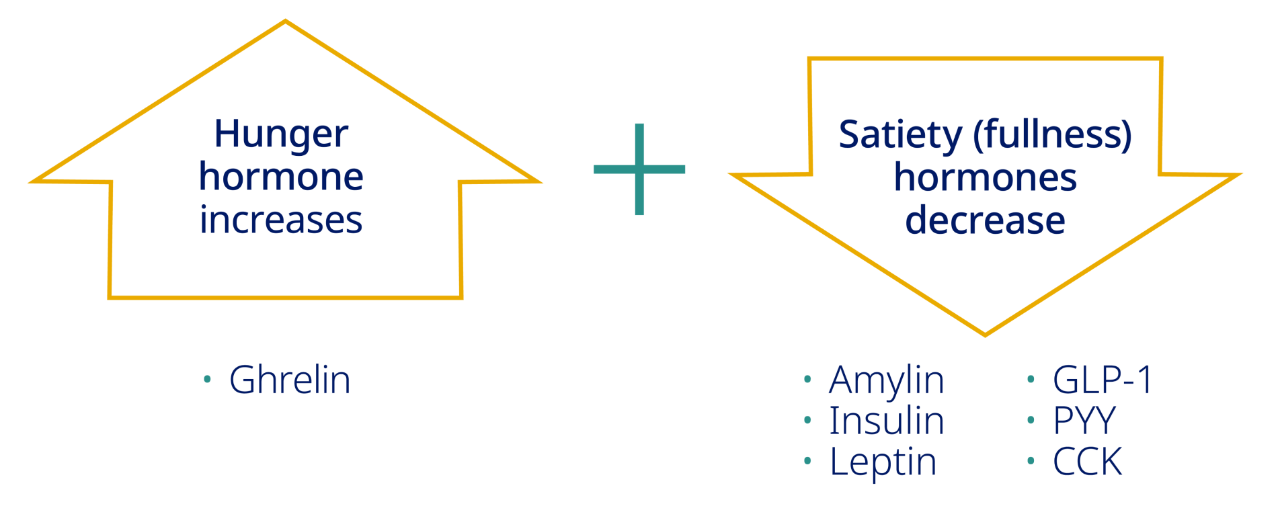
The brain plays a critical role in appetite regulation
For people with obesity trying to lose weight and maintain it, managing hunger can be a major challenge.3-8
A team of hormones from the body, including GLP-1, signal to the brain, affecting food intake7,8
AMY, amylin; CCK, cholecystokinin; GHR, ghrelin; GIP, gastric inhibitory polypeptide; GLP-1, glucagon-like peptide-1; INS, insulin; LEP, leptin; OXM, oxyntomodulin; PYY, peptide YY.
Watch how metabolic adaptation occurs
An accurate diagnosis is an important starting point for effective obesity management.9 The obesity patient example profiles available below can help

ADVOCACY AND RESOURCES
Reframing obesity management
Dr. Holly Lofton addresses the importance of proper diagnosis and what treatment can mean for patients with obesity.

DIAGNOSING OBESITY
Obesity patient example profiles
Review example profiles of patients with obesity who may be similar to patients you see in your own practice.
Metabolic adaptation, as part of the pathophysiology of obesity, must be counterbalanced by sustained efforts to maintain weight loss over an extended period9
After weight loss, metabolic adaptation leads to decreases in resting metabolic rate and lower energy expenditure2
Most of the energy expenditure comes from resting metabolic rate2,10
- In the beginning of a calorie-restricted diet, there is a reduction in energy intake that occurs more rapidly than the reduction of energy expenditure, creating an acute energy deficit that induces weight loss11
- Metabolic adaptation occurs when the decline in energy expenditure is beyond what would be expected relative to changes in body mass or composition11
- Circulating hormones (including leptin, thyroid hormones, and insulin) may mediate changes in metabolic activity11

DISEASE PROGRESSION
Obesity: lack of willpower or something more?

INITIATING A PLAN
Pharmacotherapy and weight management
References:
1. Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Eng J Med. 2011;365(17):1597-1604.
2. Lam YY, Ravussin E. Analysis of energy metabolism in humans: a review of methodologies. Mol Metab. 2016;5(11):1057-1071.
3. Yu JH, Kim MS. Molecular mechanisms of appetite regulation. Diab Metab J. 2012;36(6):391-398.
4. Austin J, Marks D. Hormonal regulators of appetite. Int J Pediatr Endocrinol. 2009;2009:141753.
5. Guyenet SJ, Schwartz MW. Regulation of food intake, energy balance, and body fat mass: implications for the pathogenesis and treatment of obesity. J Clin Endoc Metab. 2012;97(3):745-755.
6. Farr OM, Li CR, Mantzoros CS. Central nervous system regulation of eating: insights from human brain imaging. Metab Clin Exp. 2016;65:699-713.
7. Cassidy RM, Tong Q. Hunger and satiety gauge reward sensitivity. Front Endocrinol (Lausanne). 2017;8:104.
8. Druce MR, Small CJ, Bloom SR. Minireview: gut peptides regulating satiety. Endocrinology. 2004;145(6):2660-2665.
9. Garvey WT, Mechanick JI, Brett EM, et al; Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016;22(suppl 3):1-203.
10. Lam YY, Ravussin E. Indirect calorimetry an indispensable tool to understand and predict obesity. Eur J Clin Nutr. 2017;71(3):318-322.
11. Most J, Redman LM. Impact of calorie restriction on energy metabolism in humans. Exp Gerontol. 2020;133:110875.