COVID-19 and excess weight: what you need to know
Obesity is a proven risk factor for poorer COVID-19 outcomes.1,2

COVID-19 and obesity: a critical combination
Despite the decrease in COVID-19 cases, hospitalizations, and deaths, COVID-19 is still a major global health concern, especially for adults with obesity.3,4 People who are overweight may also be at increased risk for serious complications from COVID-19.2
What implications can obesity have for patients with COVID-19?
According to the Centers for Disease Control and Prevention, adults with obesity were:

~3x more likely to require hospitalization due to COVID-194
At higher risk for hospitalization, ICU, mechanical ventilation, and death due to COVID-194

Obesity was significantly associated with severe COVID-19 infection4
Obesity may be associated with an increased risk of long COVID5-7
Acute illness due to COVID-19 is not the only threat to patients with obesity. Patients with obesity may also be at a higher risk for experiencing persistent symptoms of COVID-19 infection, also known as long COVID.6 Long COVID can cause systemic inflammation, lung damage, and possibly severe physical and mental health impairments.6
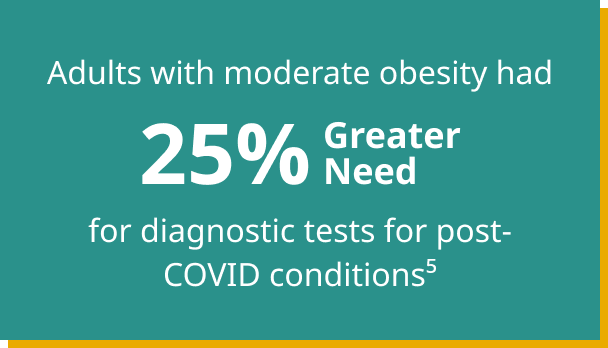
One retrospective study reported how patients with obesity fared in the time (30 days or later) following an initial positive COVID-19 test, compared with patients with a normal BMI. During the 8-month median follow-up, 44% of the 2,839 patients were admitted to the hospital.5
In this study, compared with patients who were normal weight*:
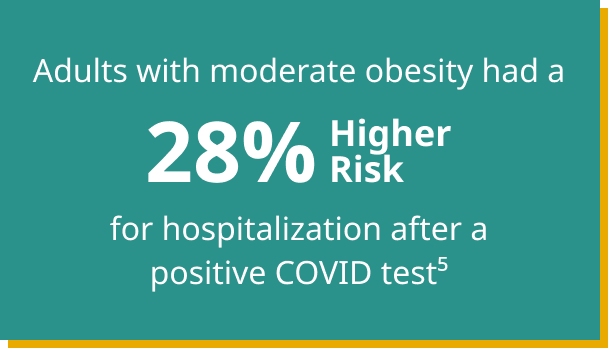
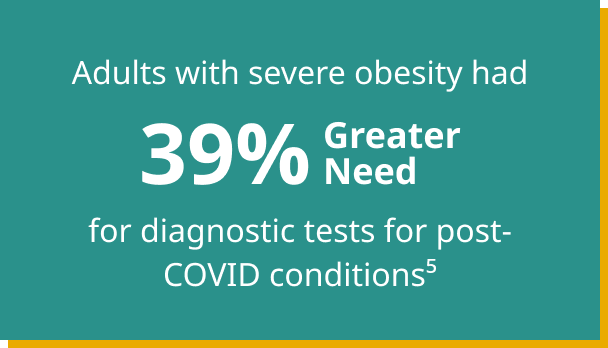
*In the analysis, normal weight was classified as BMI 18.5-24.9 kg/m2, moderate obesity BMI 35-39.9 kg/m2, and severe obesity BMI ≥40 kg/m2.
Diagnosis is the first step to treating obesity
Metabolic adaptation makes weight loss difficult
References
1. Kompaniyets L, Goodman AB, Belay B, et al. Body mass index and risk for COVID-19–related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):355-361.
2. Centers for Disease Control and Prevention (CDC). Underlying medical conditions associated with higher risk for severe COVID-19: information for healthcare professionals. Updated February 9, 2023. Accessed March 13, 2023. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html
3. Centers for Disease Control and Prevention (CDC). COVID Data Tracker Weekly Review. November 18, 2022. Accessed November 21, 2022. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
4. Centers for Disease Control and Prevention (CDC). Obesity, race/ethnicity, and COVID-19. November 18, 2022. Accessed November 21, 2022. https://www.cdc.gov/obesity/data/obesity-and-covid-19.html
5. Aminian A, Bena J, Pantalone KM, Burguera B. Association of obesity with postacute sequelae of COVID-19. Diabetes Obes Metab. 2021;23(9):2183-2188.
6. Florencio L, Fernández-de-las-Peñas. Long COVID: systemic inflammation and obesity as therapeutic targets. Lancet. Accessed October 15, 2022. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(22)00159-X/fulltext
7. Vimercati L, De Maria L, Quarato M, et al. Association between long COVID and overweight/obesity. J Clin Med. Accessed October 20, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8469321